Nutritional support is a critical aspect of the management of patients with severe burns. More than any other injury, the inflammation and catabolism associated with a burn can exacerbate nutrient deficiencies. This predisposes patients to impaired immune function, increased risk of developing infectious complications, organ failure and ultimately death.(1).
Effect of severe burns on the intestinal mucosa.
Extensive burns are associated with a massive release of inflammatory mediators into the circulation. These mediators produce an increase in vascular permeability, with extravasation of fluid into the interstitium and consequent appearance of edema.
The direct consequence of fluid extravasation is hypovolemia. The depletion of intravascular volume generates, as a response of the organism, a systemic redistribution of blood flow, increasing the perfusion of vital organs such as heart, brain, lung and adrenal glands at the expense of the decrease of the flow destined to the skin, gastrointestinal tract and kidneys (organs not essential for life).
Inadequate intestinal perfusion within the first 12 hours post-burn results in mucosal atrophy, alterations in absorption and increased intestinal permeability (loss of barrier function). Thus, toxins and microorganisms cross the wall and migrate to the portal blood circulation (bacterial translocation) leading to sepsis and organ damage.
Skeletal muscle loss in the severe burn victim
The burn patient presents with a complex neuroendocrine response that manifests itself in the clinic with hypermetabolism, hyperglycemia and a hypercatabolic state, the purpose of which is to supply the high demands for energy and substrates by the immune system and the tissues that must be repaired.
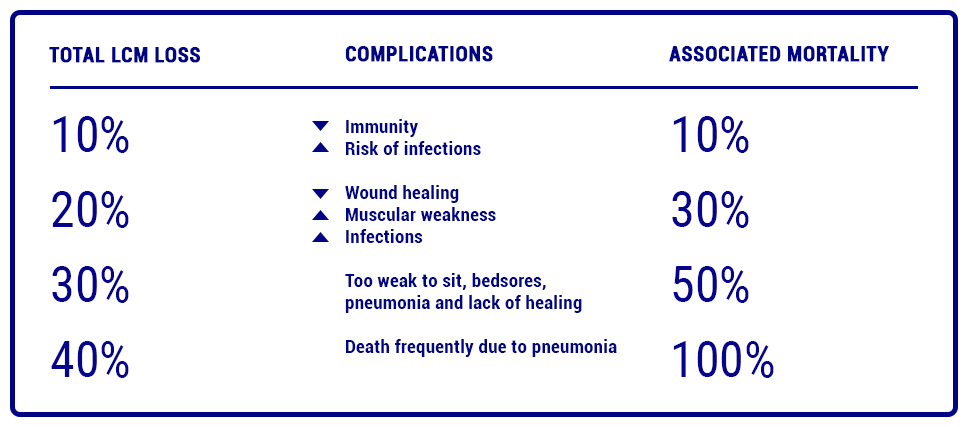
The impact that these changes in metabolism generate in the patient with extensive burns predisposes him/her to severe malnutrition with a significant loss of muscle mass, initially at the expense of skeletal muscle and later at the expense of visceral proteins.
This hypercatabolic state is associated not only with profound muscle weakness (including chest wall and diaphragm), but also with significant depression of immune function, decreased myocardial contractility, loss of intestinal barrier function, impaired wound healing, graft loss, longer hospital stay and increased mortality.
Protein requirement
Currently, protein requirements are
protein requirements are estimated at 1.5-2.0 g / kg / day for burned adults.
adults. (2)
Supplementation with this nutrient has the following objectives:
-
- Prevents the loss of lean muscle mass.
-
-
- It favors the processes of healing and rooting of grafts.
-
- Preserves immuno-competency.
Importance of Glutamine supplementation in the burn patient.
During the last decades, numerous trials have evaluated the impact of different nutritional strategies in critically ill patients and, in particular, in patients with severe burn injuries.
Glutamine is of particular interest in this respect, because of its important role in:
-
- Maintain the integrity of the small intestine.
-
-
- Being an essential nutrient for the proliferation and function of lymphocytes, neutrophils and macrophages.
-
- Its beneficial effect on healing processes.
The ESPEN nutrition guidelines recommend supplementing 0.3-0.5g/kg of glutamine per day over a period of 10 to 15 days, as soon as enteral nutrition is started. (Grade of recommendation B) (3)
Glutamine and the immune system
Although glucose is a vital metabolic and primary fuel for a large number of cells in the body, immune system cells, such as lymphocytes, neutrophils and macrophages, utilize glutamine at similar or higher rates than glucose in catabolic conditions, such as sepsis, burn recovery or surgery.
For this reason, glutamine is considered a “fuel for the immune system”, playing an essential role in cell proliferation, tissue repair process activity and intracellular pathways associated with pathogen recognition.(4)
In the presence of a severe burn, the increased demand for glutamine by the cells of the immune system, together with the increased use of this amino acid by other tissues, such as the liver (for gluconeogenesis processes), causes a deficit of this nutrient at the blood plasma level, leading to poor clinical outcomes and an increased risk of mortality. Biological rationality indicates that in these conditions its supplementation is necessary.(5)
Glutamine and the intestine
Moreover, among the various tissues that utilize glutamine at high rates, the intestine utilizes approximately 30% of total glutamine. This indicates that it is a key nutrient for this tissue.
In intestinal physiology, glutamine promotes enterocyte proliferation and regulates tight junction proteins, helping to preserve intestinal mucosal integrity and barrier function. (6) (7) (8)

Nutrisite® Restore is a food based on Whey Protein Isolate with L-Glutamine, Vitamins A and C with Zinc, indicated for the nutritional treatment of severe burns…Read more


